Exploring the Potential of the Ketogenic Diet for Brain Health
Written on
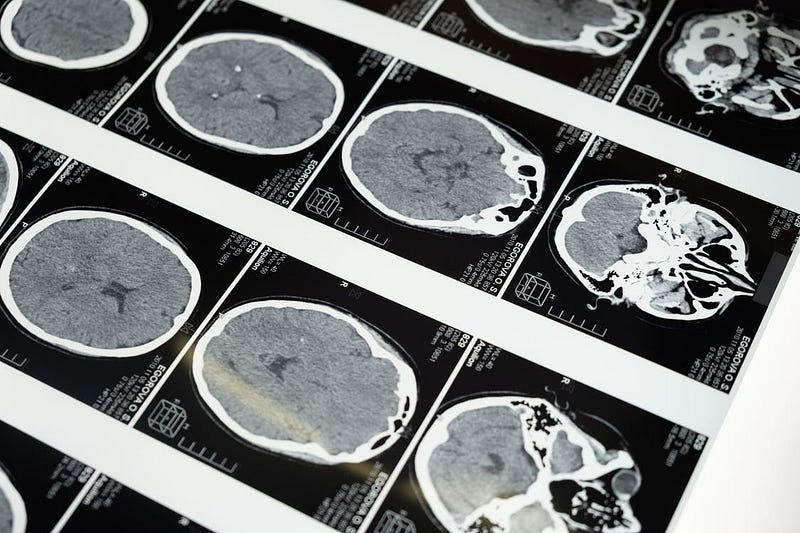
The ketogenic diet, originally developed for epilepsy treatment, has emerged as a promising approach for managing other neurological conditions. This dietary regimen shifts the body’s and brain’s energy metabolism from glucose to fat, resulting in several neurological advantages. Recent studies have highlighted its efficacy in addressing epilepsy, Alzheimer’s disease, brain tumors, and traumatic brain injury, demonstrating its potential to alleviate symptoms and possibly provide treatment. Compared to traditional medications, the ketogenic diet often presents milder side effects and offers relief for conditions unresponsive to conventional therapies, positioning it as a compelling alternative.
Historically, the ketogenic diet has been utilized since the 1920s, primarily for epilepsy. However, its benefits are now being recognized across a spectrum of neurological disorders, including brain tumors, migraines, autism, Parkinson’s disease, Alzheimer’s disease, strokes, and brain injuries. This discussion will delve into its application in epilepsy, Alzheimer’s disease, brain tumors, and traumatic brain injury while also addressing ethical and practical considerations.
The ketogenic diet is characterized by high fat intake, moderate protein, and low carbohydrates, prompting the body to rely on fat for energy instead of glucose. This mimics a fasting state, producing ketones, which are utilized by the brain as an energy source.
Compared to pharmaceutical interventions, the ketogenic diet is often preferred due to its reduced and less severe side effects. While some mild side effects, such as weight management issues, growth reduction, constipation, and kidney stones, may occur, they are typically manageable without discontinuation of the diet.
Historically, fasting has been recognized for its therapeutic potential in neurological disorders, dating back to biblical times. Hippocrates also advocated fasting for seizure management around 400 BC. The modern resurgence of interest in fasting as a treatment for epilepsy began in 1921 when Dr. Rawle Geyelin reported its success in the Medical Record. The same year, Russell Wilder noted in The Mayo Clinic Bulletin that a high-fat, low-carbohydrate diet could simulate fasting's metabolic effects, paving the way for the ketogenic diet's adoption.
Epilepsy results from excessive electrical activity in the brain, which is typically managed with antiepileptic drugs. However, around 30% of patients do not respond to these medications or other treatments, highlighting the necessity for alternative options. The ketogenic diet alters brain energy sources, effectively lowering electrical activity and reducing seizure occurrences.
In one study involving patients aged 18 and younger with structural developmental and epileptic encephalopathy, all participants showed improvements, with three achieving seizure freedom and two experiencing a 94% reduction in seizures within six months of starting the diet. Families reported enhanced quality of life, particularly in developmental and behavioral aspects.
Another investigation involving a 10-year-old with glucose transporter type 1 deficiency syndrome (Glut-1 DS) revealed that she experienced significant cognitive and seizure improvements after a week on the ketogenic diet. After three months, her processing speed and executive functioning notably advanced. Similarly, a study involving six Glut-1 DS patients found substantial neuropsychological improvements after at least six months on the diet, indicating the importance of early diagnosis and treatment initiation.
Additionally, a study on a 5-year-old with Landau-Kleffner syndrome—characterized by sudden onset aphasia and seizures—showed that while she did not respond to most antiepileptic medications, the ketogenic diet effectively controlled her seizures and restored normal cognitive function.
A broader study involving 65 children under 15 with treatment-resistant seizures found that after one year on the ketogenic diet, seizure frequency dropped significantly, from an average of 25 to fewer than two per day. Improvements were also noted in developmental and emotional functioning.
Given the challenges of adhering to the ketogenic diet, research is underway to develop medications that mimic its physiological effects, potentially providing a more convenient treatment option for drug-resistant epilepsy.
The literature indicates that the ketogenic diet is effective in treating various forms of epilepsy, significantly reducing seizures and demonstrating efficacy even in the most resistant cases through metabolic adjustments.

Research has suggested that individuals with Alzheimer’s disease exhibit hypometabolism, particularly in the hippocampus, along with mitochondrial deficiencies. A ketogenic diet might help mitigate these issues by offering neurons an alternative energy source. The initial decrease in glucose utilization is thought to contribute to Alzheimer’s progression, making this diet a potential avenue for treatment and prevention.
In one study, mice with amyloid deposits and associated memory deficits showed improved motor performance on a ketogenic diet, although cognitive function remained unaffected. Another study involving 20 adults with Alzheimer’s or mild cognitive impairment demonstrated that those consuming medium-chain triglycerides (MCTs) experienced cognitive improvements, particularly in those without the apolipoprotein E allele. Furthermore, MCT supplementation in subjects diagnosed with mild to moderate Alzheimer’s showed significant cognitive enhancements by day 45.
The ketogenic diet may effectively alleviate Alzheimer’s symptoms by providing ketones, thus bypassing glucose hypometabolism and offering neuroprotective benefits. Although research in this area is still developing, the prospects for future advancements are encouraging.
The average prognosis for glioblastoma, a malignant brain tumor, is just 18 months, underscoring the urgent need for improved treatment options. Emerging research indicates that a ketogenic diet may reduce tumor size by limiting dietary glucose availability. Cancer cells predominantly rely on glucose and often struggle to adapt to ketone metabolism, while healthy cells can easily utilize ketones. Initiating a ketogenic diet might trigger a 'sugar withdrawal,' potentially leading to increased tumor cell death.
Similar to neurodegenerative diseases, brain tumors exhibit mitochondrial deficits that hinder their ability to use ketones for energy, suggesting that a ketogenic diet could starve tumor cells, resulting in cell death.
Research on mice with gliomas indicated that those on a ketogenic diet had increased survival rates compared to those on a standard diet. When combined with radiation therapy, 81% of the mice in the ketogenic group were cured without tumor recurrence. Another study found that a ketogenic diet combined with chemotherapy resulted in reduced tumor growth and density, suggesting that metabolic therapies may enhance conventional treatments.
Utilizing metabolic alterations to manage brain tumors may present advantages over chemotherapy and radiation, which often damage healthy cells and diminish patient quality of life. Conventional treatments also provide glucose to tumor cells, potentially fueling their growth. Recent findings highlight the ketogenic diet as a viable adjunct to traditional therapies, targeting a common trait among diverse tumors, thus presenting a more efficient long-term treatment strategy.
Traumatic brain injury (TBI) is a significant cause of death and disability globally, imposing a substantial economic burden and severely affecting the quality of life for survivors. Following a TBI, the brain undergoes rapid movement within the skull, triggering a cascade of neurochemical disruptions that compromise cerebral glucose metabolism and lead to an energy crisis. This metabolic shift results in reduced glucose oxidation and ATP levels, correlating with injury severity as measured by the Glasgow Coma Scale. Mitochondrial dysfunction exacerbates secondary injury, which accounts for much of the damage following TBI, making it a target for ketogenic diet intervention.
Mitochondria can utilize ketone bodies produced through this diet as an alternative energy source, potentially enhancing energy production and neuronal survival under metabolic stress. Ketones may also exert anti-inflammatory effects, suggesting they could help prevent further concussions, as reduced energy metabolism heightens susceptibility to subsequent injuries.
A study involving juvenile rats with controlled cortical impact injury revealed that those on a ketogenic diet showed reduced oxidative stress and mitochondrial dysfunction compared to standard diet counterparts. The authors concluded that the diet's antioxidant properties contributed to early success, whereas later benefits stemmed from ketones replacing glucose as the energy source.
Another investigation assessed cognitive and motor deficits in rats after TBI. Those on a ketogenic diet performed better in beam walking and escape tasks, indicating potential improvements in cognitive and motor outcomes.
While research on the ketogenic diet's impact on cognitive and behavioral outcomes in TBI is limited, an increasing number of studies support its efficacy in mitigating secondary injury and associated symptoms, suggesting promising prospects for addressing cognitive and behavioral challenges following TBI.
The ketogenic diet has been shown to be a safe treatment approach; however, some individuals may experience gastrointestinal side effects upon initiation. Other symptoms, including brain fog, irritability, headaches, and fatigue, typically resolve within the first week.
Most studies evaluating the ketogenic diet's effects on neurological disorders have been conducted in laboratory settings, primarily on animal models, with limited human research. When human studies are available, they often involve small sample sizes or case studies without randomized designs or control groups, making it challenging to draw definitive conclusions. Additionally, since calorie restriction often accompanies a ketogenic diet, some observed benefits may arise from this factor rather than the diet itself.
Despite the varying success rates of the ketogenic diet across neurological conditions, standardizing a protocol for its implementation remains difficult. The International Ketogenic Diet Study Group has recommended assessing metabolic disorders and other complicating factors before starting the diet. Patients and families should receive thorough education on adhering to the diet and understanding its psychosocial implications. A minimum commitment of three months is suggested, with frequent follow-ups with healthcare professionals to set realistic expectations for treatment outcomes.
Conflicting evidence exists regarding the ketogenic diet's effect on children's growth, with insufficient data to draw firm conclusions. Risks of decreased bone density and weight loss due to potential vitamin D deficiencies warrant attention when implementing the diet in children.
There are considerations surrounding the integration of complementary and alternative therapies, including potential challenges with insurance coverage and the licensing of practitioners. Furthermore, the current lack of a robust evidence base for the diet's efficacy in human studies, along with the absence of specific implementation guidelines, necessitates that professionals remain informed about the literature and exercise sound judgment when recommending the diet.
In conclusion, the ketogenic diet’s effectiveness in managing neurological disorders is largely attributed to its ability to address underlying oxidative stress, inflammation, and mitochondrial dysfunction. The diet has shown promise in treating epilepsy, Alzheimer’s disease, brain tumors, and traumatic brain injury among other conditions. While research in these areas is still evolving, the ketogenic diet emerges as a safe and efficient option, offering hope to those living with these challenging disorders.
For those interested in adopting healthier habits, subscribe to my free newsletter. Each week, you'll receive a new habit to incorporate into your life, along with insights on its significance and implementation strategies. The focus is on enhancing overall health and well-being, spanning areas from nutrition and fitness to happiness and purpose.