Exploring the Connection Between White Matter Hyperintensities and Alzheimer's
Written on
Chapter 1: Understanding White Matter Changes in Aging
Aging is a natural process that brings various physical changes, particularly in the brain. As we grow older, our brains tend to shrink, and the protective layer of brain cells, known as white matter, may develop lesions. These lesions, referred to as white matter hyperintensities (WMHs), manifest as bright spots on magnetic resonance imaging (MRI).
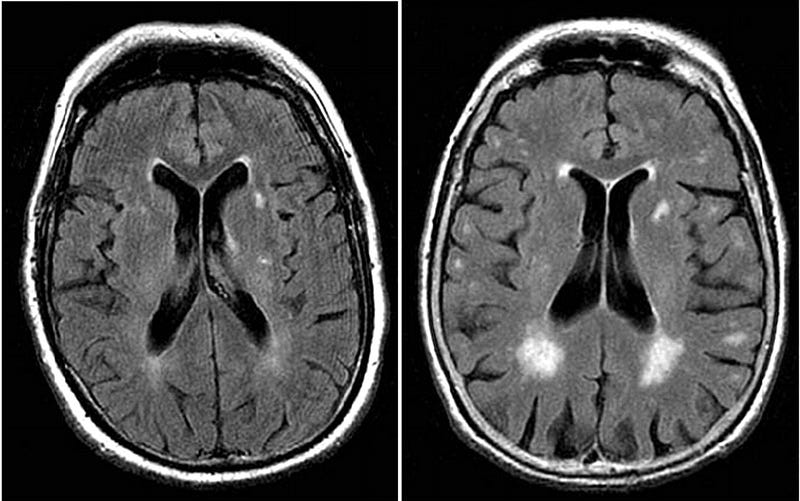
While these hyperintensities are common in older individuals without dementia, they are particularly pronounced in those with Alzheimer's disease. The presence of WMHs not only indicates a higher risk for Alzheimer's but may also accelerate the progression of the lesions themselves, creating a troubling cycle.
Section 1.1: The Relationship Between WMHs and Alzheimer’s Disease
The mechanisms behind the appearance of WMHs remain unclear. Are they solely a result of vascular problems, or do they relate specifically to the underlying processes of Alzheimer's? Recent findings suggest that both pathways may contribute to the development of these lesions.
Subsection 1.1.1: Distinct Pathways to WMHs
Evidence supports the notion that there are two separate mechanisms leading to WMHs in Alzheimer's patients. The Alzheimer-specific hypothesis posits that these hyperintensities appear earlier than in normal aging and are not solely dependent on vascular risk factors.
Research shows that WMHs are more frequently found in certain brain regions in Alzheimer's patients compared to those with typical aging. Moreover, asymptomatic individuals with genetic mutations linked to dementia exhibit a higher volume of WMHs several years prior to the onset of symptoms.
Section 1.2: Genetic Links and Biomarkers
The connection between WMHs and the APOE4 allele, which is associated with an increased risk for Alzheimer's, is significant. Genome-wide studies have also pinpointed various genes that may increase susceptibility to WMHs. Interestingly, patients with mild cognitive impairment and amyloid plaques show lower glucose uptake correlated with their WMH volume.
Chapter 2: Investigating Causes and Implications
The relationship between WMHs and Alzheimer's disease processes raises important questions regarding their origins. One theory suggests that axonal degeneration linked to neurofibrillary tangles may be responsible for the lesions, while neuroinflammation might also play a role.
While understanding the relationship between Alzheimer's, small vessel disease, and inflammation is crucial, it is equally important to consider the clinical implications of these findings.
How does knowledge of WMH origins influence treatment strategies? If WMHs are primarily due to vascular issues, managing vascular risk factors may be a key approach. Conversely, if they are tied to non-vascular Alzheimer's pathology, focusing solely on vascular health may not be as beneficial and could even result in negative outcomes.
Despite the progress in understanding WMHs, several challenges remain. The variability in WMH manifestation complicates diagnosis, and not all Alzheimer's patients exhibit significant WMH development. Each patient's disease processes may differ, further complicating assessment.
As new Alzheimer's medications become available, their impact on WMHs remains uncertain. While one might hope for positive outcomes, data is needed to clarify their effects.
Ultimately, understanding the origins of white matter lesions could lead to more targeted therapeutic options, aiding in the management of Alzheimer's disease and enhancing overall brain health.